Anxiety disorders are the most common mental health disorders experienced by children and are associated with significant negative outcomes, such as impaired academic, financial, social, and health functioning (Polanczyk et al., 2015). Half of all lifetime anxiety disorders emerge by 11 years of age, and the individuals affected are at increased risk of continued recurring anxiety and other mental health disorders later in life (Polanczyk et al., 2015; Reardon et al., 2018). Generalised anxiety disorders are defined as excessive anxiety and worry (apprehensive expectation), occurring more days than not, for at least six months surrounding a number of events. In relation to children, the anxiety is experienced as extremely challenging to control and is accompanied by at least one physical or cognitive symptom (American Psychiatric Association, 2013). Potential causes include biological, genetic, and environmental factors, as well as the parental attachment of the individual (Brown et al., 2013; Hopper, 2007; Karayağız et al., 2020).
Treatment options are available such as cognitive behavioural therapy, family-based cognitive behavioural therapy (Khanna & Kendall, 2009), treatment focused on parent–child interactions, and parental anxiety management (Cobham et al., 2010; Creswell et al., 2020). However, recent research has recognised that animals and animal-assisted therapy (AAT) can provide children with relief from anxiety symptoms as well as emotional stability in clinical and classroom settings (K. L. Anderson & Olson, 2006; Barker et al., 2015; Jones et al., 2018). Research has also shown that animals can provide socio-emotional support that can facilitate coping and resilience for children through the human–animal bond (Walsh, 2009). Pets in families offer comfort, affection, and a sense of security; therefore, these positive attributes may be transferable to a mental health clinical setting (Walsh, 2009). The therapist–client relationship may be threatening for a child, and it is possible that the presence of an animal may reduce the intensity of the therapist–client relationship and strengthen the emotional bond between the therapist and client through the sharing of the therapy animal, thereby facilitating a natural development of the therapeutic alliance (Parish-Plass, 2013).
There is growing interest in AAT in clinical practice with people who are suffering from mental health issues. For example, research has been conducted regarding AAT in the contexts of reducing anxiety levels in university students (D. Anderson & Brown, 2021) and older adults with psychiatric disorders (Berget et al., 2008; Koukourikos et al., 2019). Research has also shown the effectiveness of AAT for children with developmental disabilities regarding social interaction and participation skills (Martin & Farnum, 2002; Solomon, 2010); however, limited research has been conducted regarding the effectiveness of dog-assisted psychotherapy in reducing anxiety in children. Therefore, the aim of this literature review was to conduct a systematic literature review of studies on dog-assisted psychotherapy for children with anxiety and, in particular, to investigate the effectiveness of the presence of a therapy dog during psychotherapy sessions with children with anxiety.
Purpose Statement
The purpose of this structured literature review was to conduct a critical appraisal of the available literature relating to dog-assisted psychotherapy for children with anxiety and to investigate the effectiveness of this therapy method in reducing anxiety. The information is summarised in this paper and used to present evidence that can assist facilitation of psychotherapy practice changes and inform future research.
Research Question
Does the presence of a dog in psychotherapy sessions reduce anxiety levels in children with anxiety?
Method
The structured literature review was guided by the 12 steps recommended by Kable et al. (2012).
Databases and Search Engines
The databases included in the search were ScienceDirect, PsycInfo, and PubMed. The search was conducted during August and September 2021 with the intent to locate published peer-reviewed literature on the therapeutic benefits of involving a dog in psychotherapy sessions for children with anxiety. Google Scholar was also searched to identify any additional grey literature relevant to the research topic. To increase the chances of identifying all relevant studies, the reference lists of the retrieved articles were hand searched for papers not yet identified.
Search Limits
The limits applied to the current search were English language articles that had been published from January 2010 to August 2021. The time limit was applied to reflect the most up-to-date research literature.
Inclusion and Exclusion Criteria
To be able to represent the target population, the search was narrowed by the introduction of inclusion criteria. For this review, the inclusion criteria included the following:
-
articles whose participants included children up to the age of 18 years
-
original research articles pertaining to dog-assisted therapy or the presence of a dog in psychotherapy sessions
-
studies that had measured and reported anxiety levels in children.
Articles were excluded if they:
-
were written in a language other than English
-
focused on non-canine animals
-
focused on participants over the age of 18 years (or adults)
-
were previously published literature reviews, meta-analyses or systematic reviews, or opinion papers.
Search Terms
The search terms were developed from the research question, and alternative search terms were identified through an initial search via PubMed. The identified search terms were used to search Science Direct, PsycInfo, and PubMed focusing on the title, abstract, and body of the articles, and the Boolean operator AND was used to combine search terms, as follows:
-
children with anxiety AND dog psychotherapy
-
children with anxiety AND dog therapy AND animal-assisted therapy
-
animal-assisted therapy for children with anxiety AND canine-assisted therapy for children with anxiety.
Search Process and Search Results
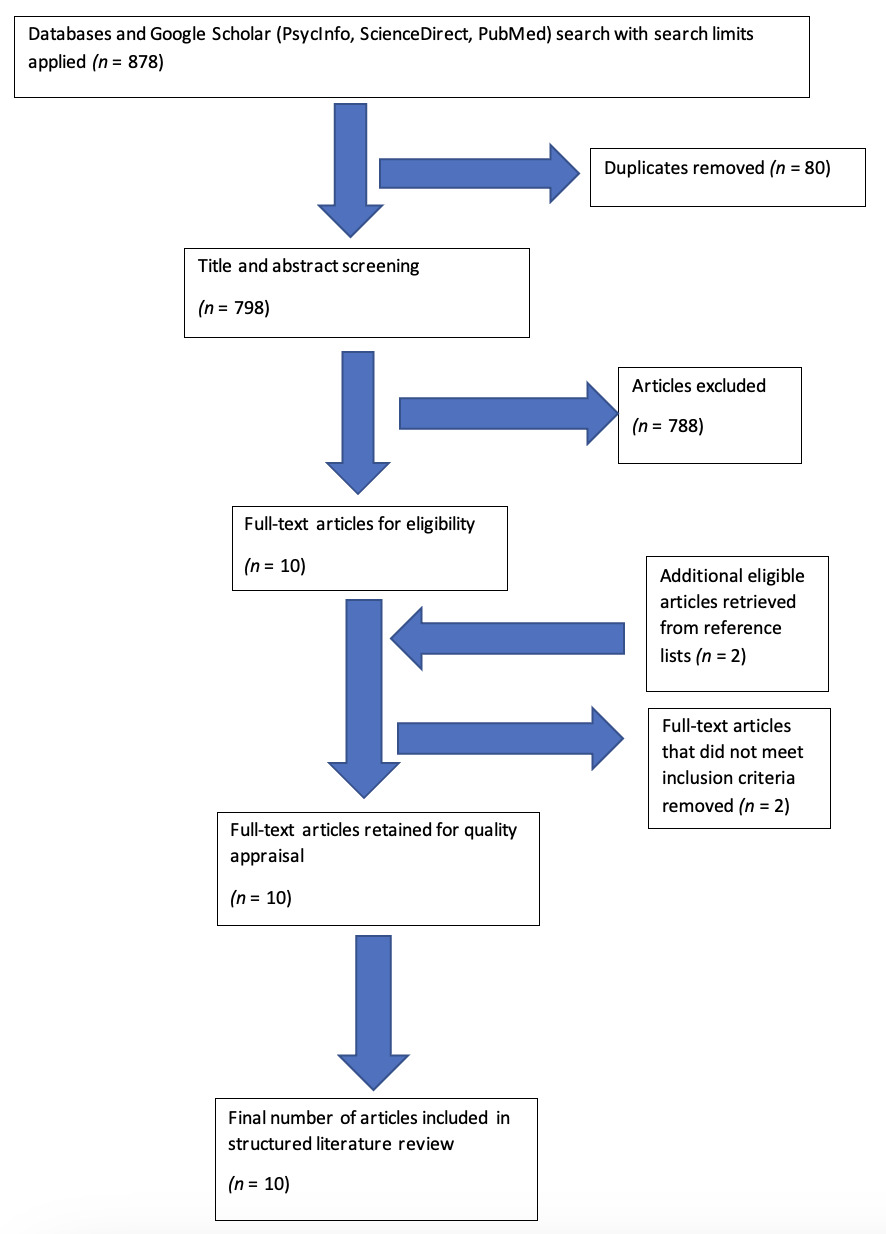
The databases were searched in sequential order. The combined search terms were used in the selected databases, and a manual search was conducted using Google Scholar search engine to identify any other relevant literature. Hand searching of the selected papers’ reference lists resulted in the retrieval of an additional two papers. Titles and abstracts were screened after duplicates had been removed, and relevance was assessed against the pre-designed inclusion criteria for the review. Studies that met or could potentially meet the inclusion criteria were retrieved in full for critical appraisal. Initially, the search returned 876 articles, and after the screening process and duplicate removal, 10 articles remained. The search process and results are presented using a PRISMA flowchart (Moher et al., 2009; see Figure 1).
Of the 10 papers, seven used a quantitative methodology and three used a mixed methods approach. Six papers were published in the United States, one in Germany, one in Italy, one in Spain, and one in Sweden. The interventions typically consisted of the presence of a dog and some level of interaction of the dog with the children in either a structured or unstructured context.
Quality of Study
The Critical Appraisal Skills Programme (CASP) tool was used to assess the full text of each selected research article for its quality according to the criteria associated with the study design and methodology (CASP, 2018). The appropriate CASP checklist was used (i.e., randomised controlled trial, case control, and qualitative checklists) to assign a score (low, moderate, high) based on the criteria. The final number of articles included for this structured literature review was 10. Seven of these papers used a quantitative methodology and three used a mixed methods approach. The summary of articles is documented in Table 1.
Results
General agreement exists in the literature that AAT can boost positive emotions and reduce anxiety levels in children. The interaction with the dogs and the unconditional acceptance received from them help reduce children’s stress and physical pain levels, as well as the stress in families and parents (Beetz et al., 2012; Branson et al., 2017; Dietz et al., 2012; Lindström Nilsson et al., 2020; McCullough et al., 2018; Stefanini et al., 2015).
Human–Animal Interactions
Animals have historically been well known for providing human companionship, being part of a therapeutic process, and having a positive impact on humans (Koukourikos et al., 2019; Walsh, 2009). Therapy dogs have been used effectively with children in hospitals and care facilities to assist with a range of disorders, abuse, oppositional behaviour, and pain management (Barker et al., 2015; Dietz et al., 2012). Children who participated in AAT were found to be more attentive, open, and alert when therapy dogs were present (Dietz et al., 2012). The human being’s relationship with animals in therapeutic interventions can provide improvements in mood, stress or anxiety, emotional stability, socialisation, and physical health factors (McCullough et al., 2018). Thus, interactions with dogs in close proximity (tactile and visual stimulation) have boosted children’s positive emotions and reduced their anxiety (Branson et al., 2017; Crossman et al., 2020).
Children’s Attachment Styles
Attachment issues have been linked with causes of anxiety in children (Hopper, 2007; Karayağız et al., 2020). Children with insecure-avoidant attachment have experienced their primary caregiver as rejecting or unsupportive; therefore, they may experience difficulties or exhibit avoidant tendencies when relating to animals, especially when stressed. Male children with insecure-avoidant or disorganised attachment benefited more from the stress-alleviating effects of interacting with a therapy dog than from interacting with a friendly adult (Beetz et al., 2012; Dietz et al., 2012). Studies also found that children with a secure attachment may benefit more from therapy dogs (Barker et al., 2015).
Hospitalisation and Environmental Considerations
Hospitalisation can be distressing to children in the context of separation from parents, painful procedures, and limited activity. The perception of pain can also be heightened by anxiety (Barker et al., 2015). Children admitted to hospitals often feel burdened, and they experience significant anxiety and negative emotions related to serious health problems and the unfamiliar environment, which negatively affect their immune function and recovery (Branson et al., 2017; McCullough et al., 2018). However, studies found that when children aged 3–18 years were admitted to hospitals, their anxiety levels were decreased by play activities that included interaction with a therapy dog (Lindström Nilsson et al., 2020; McCullough et al., 2018), and these children described positive and bright memories of their interactions with the therapy dog (Lindström Nilsson et al., 2020).
Animal-Assisted Therapy Methods and Effects
Studies that utilised AAT intervention in structured sessions with individual therapeutic goals over a 3-month period found significant positive effects on the therapeutic progress (Stefanini et al., 2015; Vidal et al., 2020). Human–animal resilience therapy (HART) combines solution-focused and canine-assisted therapies to help children with their emotional, social, and behavioural issues. A study revealed a significant difference between pre- and post-intervention stages, indicating that the HART intervention decreased anxiety, depression, and disruptive behaviours (Hartwig, 2017). A mixed methods approach study found that children reported feeling more relaxed and thinking less about their pain after they had received AAT (Lindström Nilsson et al., 2020). The AAT included a calm period, an active period involving dog tricks, followed by a period of relaxation, and each child received a stuffed toy resembling their therapy dog; the result was that the children’s fear and anxiety decreased (Lindström Nilsson et al., 2020). Children with a history of sexual abuse showed significant decreases in trauma symptoms, including anxiety, after receiving AAT (Dietz et al., 2012). However, the positive effects of AAT are not consistent. Branson et al. (2017) investigated the effects of a 10-minute interaction in which the dog was at the child’s bedside within easy reach and found that children did not demonstrate significantly larger decreases in anxiety when compared with children in the non-AAT control group.
Discussion
This literature review revealed that the presence of a therapy dog in therapy sessions or AAT created a safe environment of trust and acceptance and could reduce anxiety levels in children and adolescents (Crossman et al., 2020; Daltry, 2020). Children became more open when therapy dogs were present because they felt warmth, security, and acceptance, and they experienced a reduction in psychological distress, all of which are conditions conducive to reducing anxiety (Dietz et al., 2012; Jones et al., 2019). However, the positive effects of AAT on anxiety were inconsistent. Hartwig (2017), who used both AAT and solution-focused therapy, found that children’s levels of anxiety decreased regardless of the presence of a dog because the effects of the standalone solution-focused therapy proved sufficiently beneficial. This study was limited by a small sample size (n = 29), and differing results may arise from a larger sample size. While many cognitive and kinaesthetic activities—for example, involving a sand tray or art materials—were described in the study, no detailed specifications were provided about the type of support that the therapy dog provided. This may indicate a lack of involvement or structure for the dog’s role in the intervention.
Although AAT has been found effective at reducing anxiety levels among hospitalised children, caution should be taken when generalising these results to the wider population of children. Many challenging factors were involved with a hospital admission, such as being physically unwell, parental stress, physical discomfort levels in a foreign environment, medications taken that potentially alter mood and pain levels, and the timing of the medication taken (e.g., medication taken post-AAT). These factors may influence the psychological state of the child, and the positive effects of AAT may be heightened owing to the heightened state of anxiety. Childhood psychiatric disorders such as generalised anxiety disorder were not mentioned in Shotwell and Wagner’s (2019) study to evaluate the inclusion of animals in treatment. Autism spectrum disorders, trauma-related symptoms, and attention deficit hyperactivity disorder in children, however, were evaluated, and evidence was found to support clinicians considering the inclusion of animal-based interventions (Shotwell & Wagner, 2019).
More specific research is required to investigate AAT in different settings (e.g., classroom or outpatient therapy settings) in order to eliminate factors that may contribute to results from a hospitalised sample of children. Several studies investigated AAT’s effect on negative emotional statements, finding mostly significant decreases in anxiety after AAT in both the experimental and control groups (Holder et al., 2020). However, in another longitudinal study by McCullough et al. (2018) following the progression of paediatric oncology treatment, no significant difference was found in negative emotion between the control and the experimental group which surprised McCullough and her colleagues. Many participants in AAT studies expressed their gratitude for the intervention through non-quantitative methods such as responding to interview questions with commentary, and therefore perceived effectiveness and satisfaction is the most robustly supported result in AAT oncology studies (Holder et al., 2020). Attachment to primary caregivers demonstrated a role in the child’s relationship with a therapy dog; however, research has provided contrasting conclusions about whether children with avoidant or secure attachments benefit more from AAT (Dietz et al., 2012). It is unclear whether a linear correlation exists between attachment style and the benefits of AAT in children, so further research in this area is required to investigate the relationship and other factors involved. This information would be helpful for professionals to determine any detrimental and threatening aspects of AAT, the most suitable candidates for AAT, and the most effective way to approach AAT.
In accordance with Holder et al.’s study (2020) in which the effect of AAT on oncology patients was examined, the length of AAT or the duration of time spent with a therapy dog varied throughout the literature. These inconsistent amounts, which varied from 10 minutes to 50 minutes, may have influenced the positive outcomes of AAT. Although participants who received 10-minute AAT sessions experienced increases in their positive affect, their pre- and post-AAT differences in salivary cortisol were not significant (Branson et al., 2017). This may have been a result of brief therapy, the structure or content of the interactions, or participants’ low levels of baseline anxiety and normal levels of cortisol at the outset. Despite this, participants who received 15 minutes of AAT experienced a significant increase in positive emotions and a reduction in anxiety when compared with a control group (Crossman et al., 2020). The large degree of variation in duration and intervention method may influence the effects of AAT on children. More research is required to determine whether a particular dosage is most effective for children receiving AAT. In addition, studies varied in terms of the type of interaction (e.g., direct therapy dog interaction or guided attention towards the dog versus unstructured dog interactions), indicating potential barriers and gaps for measuring positive outcomes.
The literature has also neglected to control for factors contributing to stress relief consistently, such as family members being present, undivided attention with a caring adult, and professional and medication effects (Branson et al., 2017; Crossman et al., 2020). The studies varied in their participant selection for the baseline anxiety levels, and it was not specified whether children were diagnosed with anxiety or had undergone previous therapy for anxiety. Children who had received any other intervention method for anxiety before receiving AAT may have developed strategies for coping with anxiety and be more familiar with therapy approaches. Research conducted with children with a DSM-V diagnosis of anxiety may provide further knowledge on the effects and benefits of AAT.
Based on the research studies reviewed, a multitude of positive effects result from the presence of a therapy dog in therapeutic sessions with children. In addition to improving a child’s attentiveness and mood, when children with anxiety are misunderstood by adults or their peers, a therapy dog can provide reassurance, a sense of safety, and additional emotional support. It can be inferred that a combination approach may be most helpful in supporting children with anxiety, including both the traditional methods as well as AAT. Therefore, psychotherapists and counsellors who are interested in including a therapy dog in a therapeutic setting should feel optimistic about exploring their options, including dog therapy training to accommodate this modality, in order to provide the best support to children with anxiety. Regular clinical review with an experienced supervisor is recommended as well as ongoing monitoring of the child’s needs and therapy goals.
Conclusion
This literature review demonstrates the positive effects of the presence of a therapy dog during psychotherapy sessions for children with anxiety. The benefits include reducing anxiety levels, increasing the level of comfort or openness, and increasing positive emotions and social interaction in children with anxiety. Because of the many benefits of the presence of a dog in therapy sessions, psychotherapists and counsellors can be confident to undertake the required training and implement the necessary systems to accommodate a therapy dog in a psychotherapy or counselling session. The therapeutic setting and the child’s needs will vary, and therefore the individual therapist will need to make judgements regarding the nature of the session and whether the sessions should include active and direct contact or more indirect contact with the therapy dog.
Limited research has been conducted on children in settings other than hospital settings; therefore, it is challenging to understand and assess the effectiveness of AAT in other contexts, such as therapy, home, or school settings. While strong evidence exists to support the benefits of AAT, more research is required regarding the clinical implications of the nature of the AAT, type of AAT intervention, and length of AAT.